Nobel laureates extolled the potential of mRNA

The discoveries of Katalin Karikó and Drew Weissman made possible the first COVID-19 vaccine. But it was just one of the many things that can be done with mRNA, explained the Nobel laureates in Physiology or Medicine in their Nobel lectures.
Once the audience in a packed Aula Medica had been welcomed by Karolinska Institutet president Annika Östman Wernerson, Professor Olle Kämpe introduced the Nobel laureates.

"I’ve never lectured to so many people," said Katalin Karikó who was the first of the two to speak.
She talked about the history of mRNA therapy and her own contributions to the research, as well as her less successful career moments. The mRNA molecule, which acts as a protein recipe in the body, was discovered in 1961.
It took 60 years for the first mRNA therapy to be approved, in the form of the first COVID-19 vaccine.
One milestone was reached in 1984, when researchers managed to synthesise mRNA in a test tube. This piqued the interest of Katalin Karikó, who had been researching mRNA at Szeged University in Hungary since 1978.
Many researchers had ideas about how mRNA could be used, including for the development of influenza and cancer vaccines.
"But most of them didn’t continue to publish later on, because there was a problem," she explained. "The amount of protein produced was too small and they had trouble obtaining further funding."
After moving to the USA in the mid-1980s, she eventually found work in a laboratory at Pennsylvania University, where she remained for 17 years. But like her colleagues in the mRNA field, she struggled to obtain grants.
"I did the work with my own hands," she said, citing the defrosting of freezers as one of her duties.
An encounter with destiny at the photocopier
In 1997 she happened to meet university colleague Drew Weissman in a queue for the photocopier. Their chat blossomed into a collaboration.
"He was interested in developing HIV vaccines and told me he was working with dendritic cells. I didn’t know what they were, but I learned immunology from him."
Together, they demonstrated that mRNA is able to activate the dendritic cells, and realised that it could work as a vaccine – but it caused an inflammatory reaction that they needed to learn more about first. Finally, they worked out that the inflammation could be avoided by modifying one of the components of the mRNA molecule, the nucleoside uridine.
Come 2012, much had fallen into place. They had shown by then that mRNA injected into mice produced a working protein without causing inflammation.
"And that was, again, when I lost my position," said Dr Karikó.
Fortunately, she heard about the then not-so-large company BioNTech, and continued her work there. The company went on to become one of the first to succeed in developing an mRNA vaccine against COVID-19, but Dr Karikó left that fact aside in her lecture, focusing instead on the general advantages of using mRNA to produce proteins for many different types of drug and vaccine.
"250 mRNA-based therapies are now being clinically tested," she said and handed over to Drew Weissman, whose lecture centred on the current state of affairs and the future of the research field.
mRNA makes many dreams come true
Drew Weissman began by thanking the Nobel Assembly and all the researchers in the audience.
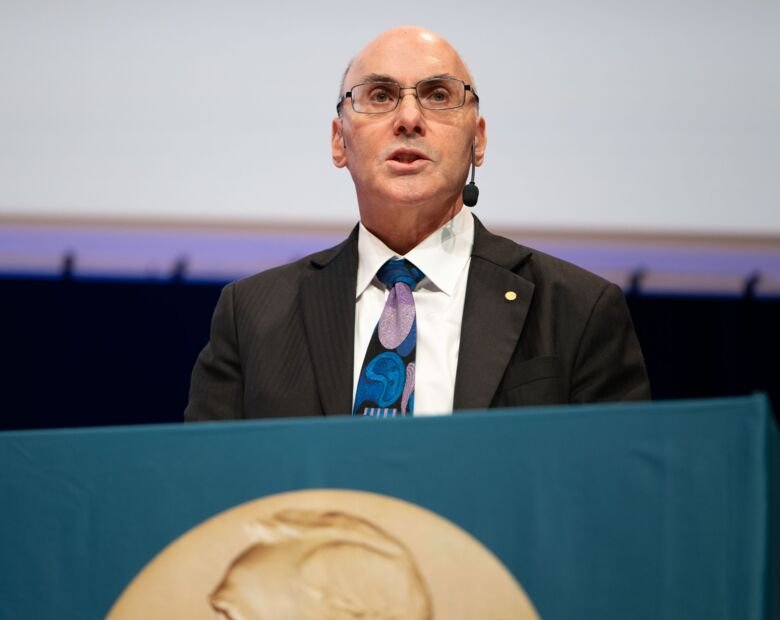
"Most of all, I have to thank Katie, because Katie is the person who introduced me to RNA," said Drew Weissman and explained that he was a researcher whose many dreams had come true thanks to mRNA and his collaboration with Katalin Karikó.
He talked about how mRNA vaccines can be used for influenza, a disease that changes every year, which means that the vaccine has to keep up.
"Which unfortunately means that we have to guess what the next year’s virus will look like," said Dr Weissman. "Sometimes we get it right, but often we don’t."
Different kinds of vaccine have been used for influenza, but when Dr Weissman and his colleagues tested mRNA on animals, they found that it produced extremely high levels of antibodies. The results were so strange that one of his collaborators burst into his office and accused him of faking the samples.
"I explained to him that they were the real results," he said.
It later transpired that the lipid nanoparticles, the tiny fat bubbles used to deliver the mRNA molecules into the body, act as a so-called adjuvant that triggers the immune response.
Protection against different types of influenza
One advantage of mRNA vaccines is that they can quickly be adjusted to the target molecule. They can also be designed to protect against different types of influenza, including viruses that risk jumping from animals to humans and causing a pandemic.
Such universal influenza vaccines are now being tested clinically on humans, Dr Weissman explained. One of the vaccines he is developing, which has proved effective on animals, is loaded with 20 different RNA molecules to provide protection against all subgroups of influenza.
Dr Weissman described a future in which many of the routine vaccinations given to children can be replaced by a handful of mRNA vaccinations against many different diseases.
“It would greatly simplify parents' lives. And it would drive pharmaceutical executives insane because they would lose all the vaccines they were producing,” he said. “I don't know if it will ever happen, but we can dream about it.”
Another application is a cancer vaccine that can be given to people with an inherited predisposition to cancer before they develop the disease.
"We know that cancer cells can start to appear 5 to 10 years before symptom-producing tumours develop," said Dr Weissman, and explained that a regularly administered vaccine that can wipe out all mutated calls could prevent cancer developing.
A huge potential for vaccine development
Finally he talked about the potential of mRNA therapy in which lipid nanoparticles containing mRNA are designed to target a certain location in the body – such as the dormant immune cells in which the HIV virus hides.
Another application is immunological therapy using so-called CAR-T cells. The therapy is currently expensive and requires the removal of T cells from the body, their cultivation and loading with antibodies against tumour cells, and their reintroduction into the patient. With lipid nanoparticles and mRNA, the CAR-T cells can instead be created internally, Dr Weissman explained.
Dr Weissman believes that mRNA therapy has huge potential not only for vaccine development but also for curing cancer and genetic diseases – and in the future gene therapy need not be a burden for the patient, as one injection will suffice.
"“I like to joke with my lab staff that we haven’t thought of everything that can be done with RNA yet, and that that’s now their job. I've done my job,” he said.
Text: Ola Danielsson







