New tools to study the origin of embryonic stem cells
Researchers at Karolinska Institutet have identified cell surface markers specific for the very earliest stem cells in the human embryo. These cells are thought to possess great potential for replacing damaged tissue but until now have been difficult to distinguish from classical embryonic stem cells. The study is published in the prestigious journal Cell Stem Cell.
During the first week of fertilisation, the embryo grows from a single cell into a blastocyst, a hollow cluster of a few hundred cells. The blastocyst then attaches itself to the wall of the uterus (implantation), and for a limited period from fertilisation to a few days after implantation the embryo contains pluripotent stem cells. These cells can develop into all the body’s cell types and are therefore of considerable interest to the field of regenerative and reparative medicine.
Two stages for human pluripotent stem cells
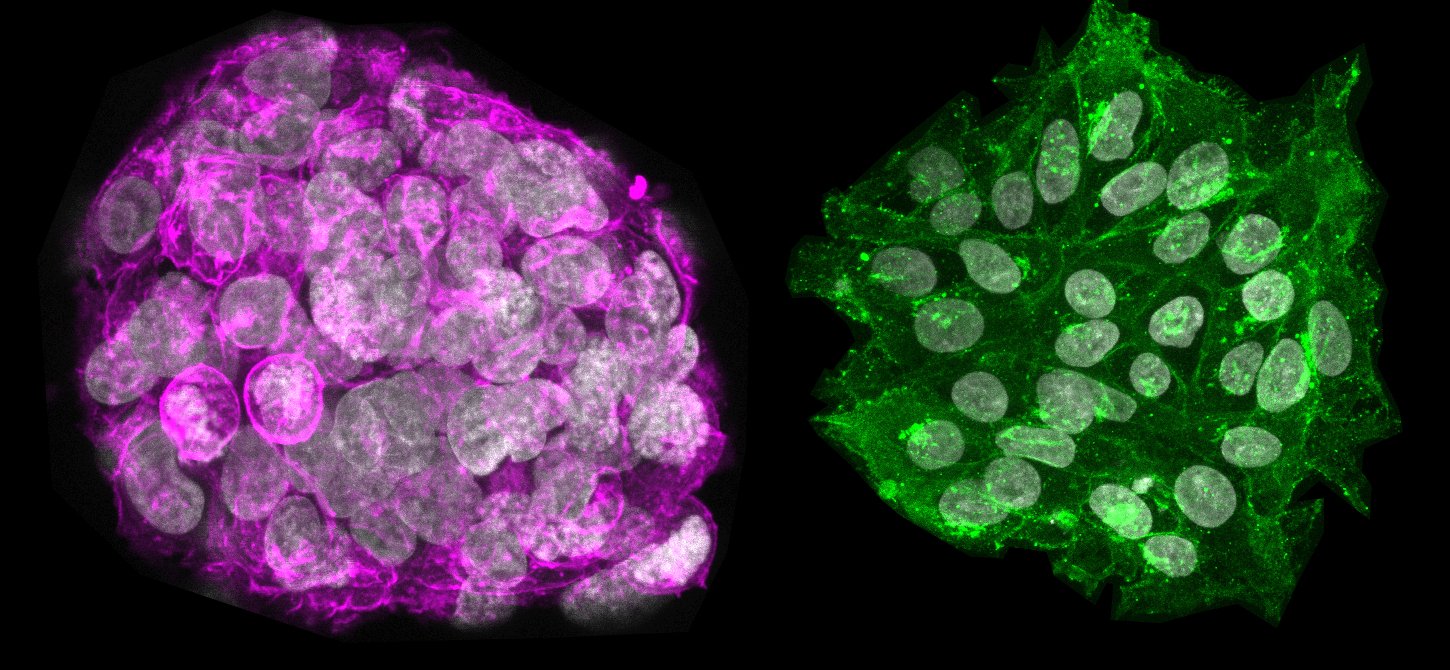
A few years ago, it was discovered that there are two stages for human pluripotent stem cells, corresponding to the pre-implanted and post-implanted embryonic cells. Although the classical stem cells used in regenerative medicine are isolated from the pre-implanted embryo, they have adopted a mature stage that is most likely more similar to a post-implantation embryo. A new type of pluripotent cell that genuinely corresponds to the more immature, pre-implantation stage has been identified and can now be cultivated in the laboratory. These immature stem cells are of great scientific interest since they are believed to have the potential to build certain cell types that are difficult to obtain from the classical stem cells, and they may also be easier to cultivate and manipulate in the laboratory.
 Fredrik Lanner’s research team at Karolinska Institutet and their colleagues in Peter Rugg-Gunn’s team at Cambridge’s Babraham Institute in the UK have now developed a tool for separating the two stem cell states. They have screened combinations of antibodies that bind to specific proteins on the surface of the immature and mature stem cells and that can be used for flow cytometry, a common laboratory technique for sorting cells.
Fredrik Lanner’s research team at Karolinska Institutet and their colleagues in Peter Rugg-Gunn’s team at Cambridge’s Babraham Institute in the UK have now developed a tool for separating the two stem cell states. They have screened combinations of antibodies that bind to specific proteins on the surface of the immature and mature stem cells and that can be used for flow cytometry, a common laboratory technique for sorting cells.
Benefits future stem cell research
“We’ve not had cell surface markers for the different stem cell states before, which has made it hard to study them,” says Fredrik Lanner, Assistant Professor at Karolinska Institutet’s Department of Clinical Science, Intervention and Technology. “We now have a simple tool for identifying and sorting the cells, which benefits future stem cell research and basic research on early embryonic development.”
Mature embryonic stem cells cultivated in the laboratory can, under the right conditions, be backed up in their development to the more immature stem cell type. The researchers tested their technique on such cultivated stem cells of both a mature and immature type, and on donated human embryos left over from IVF treatments. As expected, only the immature stem cell type was identified in such pre-implanted embryos, which indicates that the antibodies are highly specific.
A highly critical time for the embryo
“It is at the point of implantation that the stem cells go through this change and ‘mature’, which is also a highly critical time for the embryo,” says Dr Lanner. “These cells are therefore also of interest to infertility research.”
The study was financed by several bodies, including the Swedish Research Council, the Ragnar Söderberg Foundation, the Swedish Foundation for Strategic Research, the Knut and Alice Wallenberg Foundation, the Centre for Innovative Medicine (CIMED) and the Ming Wai Lau Centre for Reparative Medicine.
Publication
Comprehensive Cell Surface Protein Profiling Identifies Specific Markers of Human Naive and Primed Pluripotent States
Amanda J. Collier, Sarita P. Panula, John Paul Schell, Peter Chovanec, Alvaro Plaza Reyes, Sophie Petropoulos, Anne E. Corcoran, Rachael Walker, Iyadh Douagi, Fredrik Lanner, Peter J. Rugg-Gunn
Cell Stem Cell, online 23 March 2017, doi: 10.1016/j.stem.2017.02.014
