New ways to study how cancer arises

In an interdisciplinary study combining stem cell biology and tumor biology, researchers from Karolinska Institutet (as well as Uppsala and Lund University, together with researchers in Canada, Germany and France), have succeeded in creating a new type of stem cell models for studies on cancer of the brain. The study was recently published in PNAS.
What are the main results of the study?

“We have created a new type of model for Medulloblastoma which is one of the most common forms of brain tumors that affect children. With current treatment, about 60% of the children affected survive”, explains Margareta Wilhelm, researcher at the Department of Microbiology, Tumor and Cell Biology.
The treatment is often very tough and consists of surgery, radiation and chemotherapy, which can result in side effects in the form of cognitive problems, endocrine disorders, as well as increased incidence of secondary cancer later in life, which emphasizes the importance of developing effective treatments that do not harm the healthy part of the brain.

"In order to identify and test new treatments for this form of childhood cancer, we need to develop models that mimic the onset and growth of the disease," says Anna Falk, a researcher at the Department of Neuroscience.
How was the study conducted?
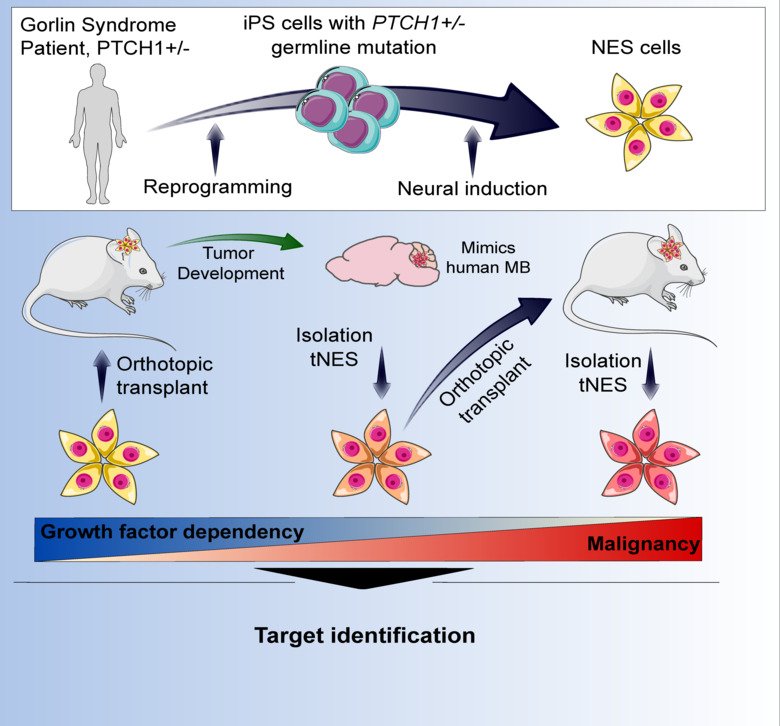
“We have developed a model for Medulloblastoma by reprogramming skin cells from Gorlin’s syndrome patients who carry a hereditary mutation in the PTCH1 gene - one of the most common mutated genes in Medulloblastoma - to become pluripotent stem cells and further to become neural stem cells, believed to be the cell of origin for Medulloblastoma," Anna Falk continues.
"We show that transplanted patient neural stem cells form tumors in the cerebellum of mice, while cells from healthy individuals cannot," says Margareta Wilhelm.
The tumours that are formed are similar to those developed in Medulloblastoma patients and the researchers show that their model can be used to understand how the cancer starts and thereby find new therapy goals.
This study is unique because it connects two different research fields where the best and newest techniques from both fields are used. The study is funded by the Swedish Childhood Cancer Fund (Barncancerfonden), the Swedish Cancer Society (Canderfonden) and the Swedish Research Council.
Publication
Modeling SHH-driven medulloblastoma with patient iPS cell-derived neural stem cells
Susanto E, Navarro AM, Zhou L, Sundström A, van Bree N, Stantic M, Moslem M, Tailor J, Rietdijk J, Zubillaga V, Hübner JM, Weishaupt H, Wolfsberger J, Alafuzoff I, Nordgren A, Magnaldo T, Siesjö P, Johnsen JI, Kool M, Tammimies K, Darabi A, Swartling FJ, Falk A, Wilhelm M
PNAS, 2019-20521R
