New strategy to preserve insulin-producing cells in diabetes
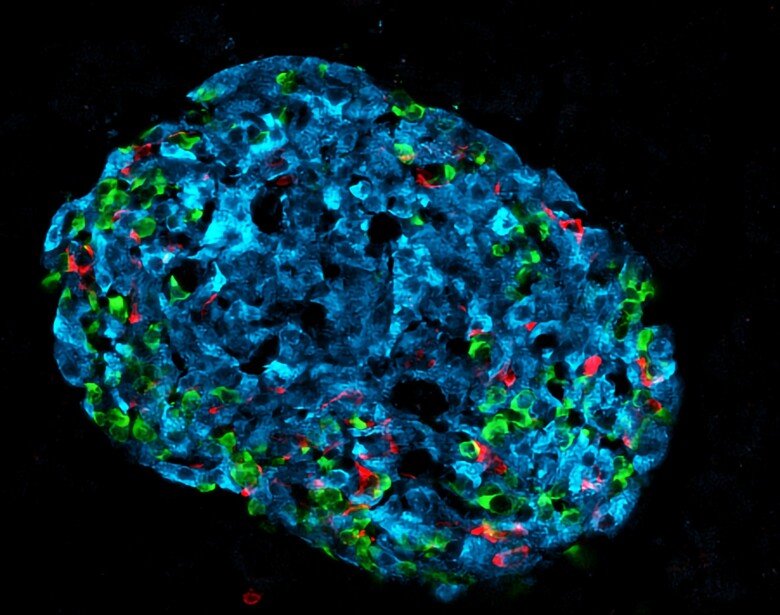
High blood glucose is responsible for several complications in type 1 and type 2 diabetes. Researchers at Karolinska Institutet have identified a new antidiabetic substance that preserves the activity of insulin-producing beta cells and prevents high blood glucose in mice. The study is published in the journal Science Translational Medicine.

Although several families of glucose-lowering agents are currently used in diabetes therapy, none of them can stop or reverse the progression of the disease. Maintenance of adequate beta cell activity is essential to prevent the progression of type 1 and type 2 diabetes.
“In diabetes, beta cells are challenged to produce high amounts of insulin,” says the study’s first author Erwin Ilegems, senior researcher at the Department of Molecular Medicine and Surgery, Karolinska Institutet. “Our study shows that this leads to a hypoxic state that increases the levels of HIF-1a protein, which in turn reduces beta cell activity. By treating diabetic mice with the HIF-1a inhibitor PX-478 we successfully decreased their blood glucose levels.”
Repurposing an anti-cancer drug
HIF-1a (hypoxia-inducible factor-1a) regulates the response to hypoxia. The discovery of HIF-1a was awarded the Nobel Prize in Physiology or Medicine in 2019 and this protein is involved in many different diseases. The HIF-1a inhibitor PX-478 has already been tested in phase I clinical trials as an anticancer drug and was well tolerated in these patients.
In collaboration with Professor Jorge Ruas’ research group at the Department of Physiology and Pharmacology at Karolinska Institutet, the authors could demonstrate that the antidiabetic effect of PX-478 was mainly due to improved pancreatic beta cell activity.
Since it is well established that the production of insulin decreases during the progression of diabetes, therapeutic strategies have so far mostly focused on improving the insulin production of beta cells. However, this approach has not been as successful as initially predicted.
“Current therapies targeting beta cells have only a temporary positive effect on insulin secretion,” says the study’s last author Per-Olof Berggren, professor at the Department of Molecular Medicine and Surgery, Karolinska Institutet. “In the long-term, these drugs lead to beta cell exhaustion.”
Long-term treatment of diabetes

Unlike other treatments, PX-478 ameliorates beta cell activity without amplifying insulin secretion. The researchers therefore believe that it can prevent the exhaustion of beta cells and thus be more efficient in the long-term treatment of diabetes.
“We are now planning to further investigate the translatability of our findings to hopefully pave the way for future clinical trials,” says Teresa Pereira, researcher at the Department of Medical Cell Biology, Uppsala University (formerly employed by Karolinska Institutet), who is co-last author of the study. “We will start by investigating the impact of PX-478 on human pancreatic beta cell activity by using ‘humanised’ diabetic mice.”
This work was supported by funding from Karolinska Institutet, the Swedish Research Council, the Novo Nordisk Foundation, the Swedish Diabetes Association, the Family Knut and Alice Wallenberg Foundation, Diabetes Research and Wellness Foundation, the Jonas & Christina af Jochnick Foundation, the Family Erling-Persson Foundation, Berth von Kantzow's Foundation, the Skandia Insurance Company, Ltd., the European Research Council, the European Union's Seventh Framework Programme, and the European Diabetes Research Programme in Cellular Plasticity Underlying the Pathophysiology of Type 2 Diabetes. Teresa Pereira has filed a patent entitled “Treatment of diabetes”, and co-author Burcak Yesildag is an employee at InSphero AG. All other authors report no competing financial interests.
Publication
”HIF-1alpha inhibitor PX-478 preserves pancreatic beta cell function in diabetes”. Erwin Ilegems, Galyna Bryzgalova, Jorge Correia, Burcak Yesildag, Edurne Berra, Jorge L. Ruas, Teresa S. Pereira, Per-Olof Berggren. Science Translational Medicine, online 30 March 2022, doi: 10.1126/scitranslmed.aba9112.
