New strategy can improve cell therapy against cancer
Researchers at the Center for Infectious Medicine at the Department of Medicine, Huddinge have developed a new strategy that can make cell therapy against cancer work longer in patients. The results are published in the journal Cell Stem Cell.

What does your publication show?
“Our publication shows that we can learn from nature: it is well known that viruses and tumours use strategies to escape from our immune system. We saw these virus or tumour escape attempts as blueprints and used state-of-the-art genetic engineering technology to apply them to cell therapy against cancer”, says Quirin Hammer, first author of the study and research team leader at the Center for Infectious Medicine (CIM) at the Department of Medicine, Huddinge.
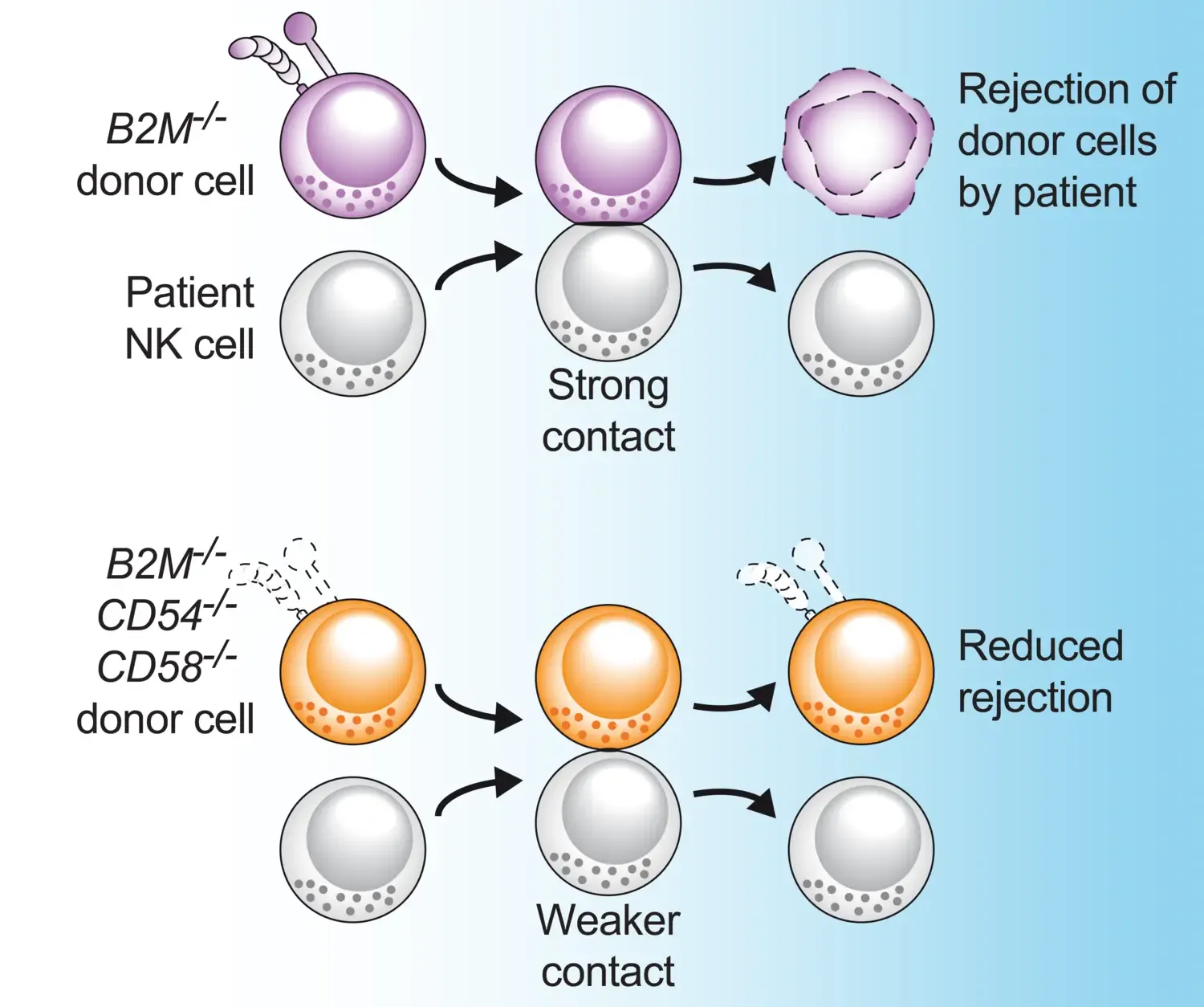
“So-called allogeneic cell therapy, where cells from healthy donors are used in an off-the-shelf setting to treat patients with cancer, has great potential to become an affordable and broadly applicable therapy for many patients. However, it currently suffers from some shortcomings. One is that if cells from a donor are infused into a patient as a "living drug", then the immune system of the patient can respond and destroy the infused cells. Our strategy aims at reducing the contact between the donor cells and the patient’s immune cells and can therefore be used to reduce the rejection by the patient's immune system. This leads to an extended persistence of the donor cells in the patient.”
Why are the results important?
“We think that they are important because they address a central limitation of allogeneic cell therapy. Our strategy could help overcoming rejection of therapeutic donor cells by the patient´s immune system and may improve the efficacy of allogeneic cellular therapies against cancer and maybe even against other diseases.”
How did you perform the study?
“We combined work in cell culture with animal models of immune rejection and used state-of-the-art genetic engineering including the so-called "gene-scissors" CRISPR/Cas9 to modify donor cells. Being able to test our concept in several different settings was made possible through collaboration with numerous researchers here at the NextGenNK competence center as well as scientists from Oslo and New York City. We also worked in partnership with the US-based company Fate Therapeutics. These diverse collaborations were fundamental to the success of our study.”

What is the next step in your research?
“The current results are pre-clinical, so a logical and exciting next step would be to work towards clinical implementation of the strategy. It will also be interesting to combine our strategy with additional ones to make it even more efficient.”, says Karl-Johan Malmberg, last author of the study and group leader at CIM, co-director of NextGenNK, and director of the Precision Immunotherapy Alliance (PRIMA) at the University of Oslo, Norway.
EU Horizon 2020 under Marie Sklodowska-Curie grant agreement No. 8382909, Felix Mindus contribution to Leukemia Research, Region Stockholm, The Swedish Research Council, The Swedish Children´s Cancer Society, Cancerfonden, SSF, KAW, The Research Council of Norway, PRIMA, and many more.
Karl-Johan Malmberg is a consultant and has research support from Fate Therapeutics. Karl-Johan Malmberg and Quirin Hammer are consultants at Vycellix. All relationships have been approved by Oslo University Hospital, University of Oslo, and Karolinska Institutet.
Publication
Check out @QuirinHammer on X (formally Twitter) for a "tweetorial" on the study.
