Grant awarded to Susanne Nylén group for research on skin-related neglected tropical diseases
Susanne Nylén at the Department of Microbiology, Tumor and Cell Biology at KI, is leading a project that has been awarded a four-year grant from the Dutch foundation Dioraphte for research on the pathogenesis of post-kala-azar dermal leishmaniasis (PKDL) and leprosy. The total amount awarded is 850 000 euros.

What is PKDL?
“Post-kala-azar dermal leishmaniasis (PKDL) and Leprosy are two skin infections that affect the poorest populations causing disfigurement, scarring, and stigmatization with devastating and long-lasting effects on the quality of life for those affected. PKDL is a dermal sequela that can present several years after the therapeutic cure of visceral leishmaniasis (VL), a life-threatening disease caused by the parasitic protozoa Leishmania donovani. Patients with PKDL do not always actively seek treatment, as the skin pathology can be confused with another skin NTD, namely Leprosy – a chronic bacterial disease caused by Mycobacterium leprae, that has been feared by many and historically has led to ostracization in most societies. Notably, there are still more than 200,000 new leprosy cases reported every year, most in India”, says Susanne Nylén, principal researcher at the Department of Microbiology, Tumor and Cell Biology at Karolinska Institutet.
What will your project focus on?
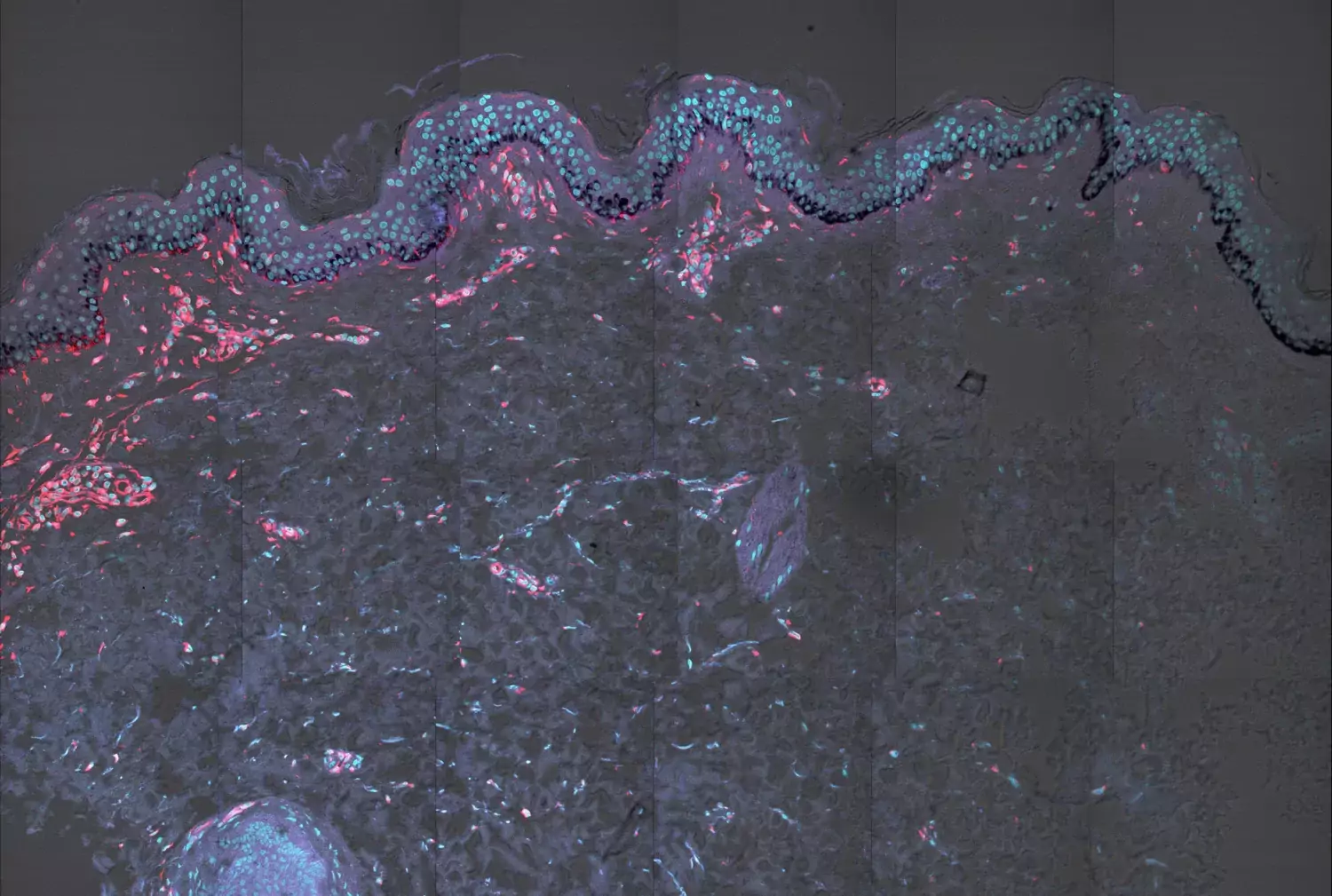
“Both PKDL and leprosy can present with macules and/or nodular lesions. The macular variant of PKDL is akin to the tuberculoid form of leprosy, in that both present with loss of skin pigment (melanin), a low pathogen burden, and minimal infiltration of immune cells. Importantly these forms are difficult to treat. On the other hand, the nodular variant of PKDL shares similarities with the lepromatous form of leprosy in that both have a high pathogen load, a considerable degree of immune cell infiltration and respond well to treatment. In the absence of animal models, knowledge about the development of PKDL and leprosy remains limited”, Susanne says.
“We want to understand if responses required for pathogen control are concomitant or independent from those causing de-pigmentation. Furthermore, reasons for increased pathogen burden in nodular/polymorphic PKDL and lepromatous leprosy need to be understood to facilitate the development of new treatments. Together, the proposed analysis of human samples using cutting-edge technologies will advance our understanding and fill knowledge gaps on immune regulation across the disease spectra of PKDL and Leprosy.”
Who is taking part in the study?
“The project builds on existing partnerships and collaborations between scientists and clinicians in India, Australia, Denmark, Sudan and the UK. The clinical research will originate from three centers in India, along with using archived samples from Sudan”, Susanne explains.
Which patient groups will benefit from your research?
“PKDL and Leprosy are stigmatizing skin diseases that can cause ostracization and have a major impact on the quality of life for the poor people affected. By applying leading technology and advanced approaches to these NTDs, insights into processes underlying pathology and disease evolution will be made, which in turn can pay the way for new diagnostics and therapeutic strategies”, says Susanne.
“Since PKDL cases harbor parasites in their skin, they are potential disease reservoirs for L. donovani transmission and can when bitten by sandfly vectors contribute to upholding the VL transmission cycle. To aid VL elimination campaigns, it is important to effectively treat PKDL cases, yet these treatments are long-term, coupled with substantial side effects, and safer treatments are urgently needed. Therapies targeting the local immune responses can be a way forward but require an increased understanding of the overall ‘immune landscape’.”
Full title of the project
“Understanding the link between immune pathology, hypopigmentation and pathogen control in Post kala-azar Dermal Leishmaniasis (PKDL) and Leprosy”
Co-Investigators
Prof. Mitali Chatterjee, Institute of Postgraduate Medical Education & Research (IPGMER), Kolkata, INDIA
Dr. Rajiv Kumar, Centre of Experimental Medicine and Surgery (CEMS), Institute of Medical Sciences (IMS), Banaras Hindu University, Varanasi, INDIA
Prof. Shyam Sundar, Director-Kala-azar Medical Research Centre (KAMRC) Muzaffarpur, Bihar, INDIA & Distinguished Prof., Department of Medicine, IMS, BHU.
Prof. Paul Kaye, York Biomedical Research Institute, Hull York Medical School, University of York, York, UK
Prof. Christian Engwerda, QIMR Berghofer Medical Research Institute, Brisbane, AUSTRALIA,
Prof. Liv Eidsmo, Leo Foundation, Skin Immunology Center (SIC), Univ. of Copenhagen, DENMARK
Prof. Ahmed M Musa, Inst. of Endemic Diseases, University of Khartoum, Khartoum, SUDAN
Prof. Nilay K Das, Dept. of Dermatology, College of Medicine, Sagar Datta Hospital, Kolkata, INDIA
