Conflict alone is a poor indicator of child health in the Democratic Republic of Congo

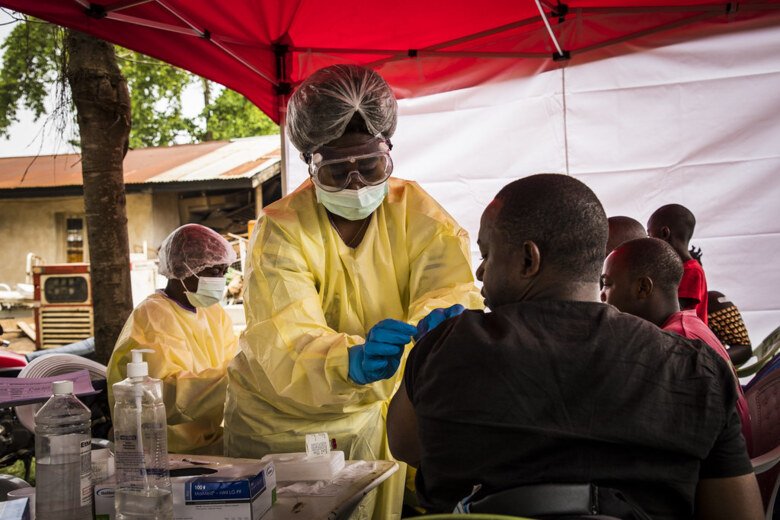
Conflict causes deaths and injuries, as well as health consequences from the displacement of populations, breakdown of health services and an increased risk of disease transmission. But in DRC that has suffered from conflict and instability for decades, conflict alone is a poor indicator for child health. In his study, Mattias Schedwin, compares coverage of key child health policy indicators across provinces in DRC and their association with child mortality and level of conflict in the country.

A long and inequitable way to reach good health for all
"In our study, we have compared indicators relevant to child mortality, such as vaccination status and access to correct treatment for diarrhoea, between the 26 provinces in the Democratic Republic of Congo (DRC), the second largest country in Africa, and looked at how they were associated with child mortality", says doctoral student Mattias Schedwin who is based in Kinshasa.
Coverage of these indicators was found to differ greatly between the provinces, for example, the Pneumococcal conjugate vaccine varied from 9% coverage in the province with the lowest rate to 90% in the highest. A simple thing as having access to water and soap for washing your hands varied from 0,5% to 70% in coverage rate. This suggests that children’s prerequisites for survival vary considerably between the DRC provinces which is yet an additionaldemonstration that great inequity in child health not only occurs between countries but also within countries.
Children more likely to be covered by health services in conflict areas
Mattias Schedwin has also looked at the likelihood of being covered by key child health policy indicators, comparing if a child lived in a conflict-affected province or not. Perhaps unexpectedly, he saw that overall children in provinces affected by conflict were more likely to be covered by these indicators. However, conflict-affected provinces also had the highest as well as the lowest indicator coverages.
An estimated 40% of DRC’s health care is financed from people spending out of pocket which is particularly problematic as three quarters of the population live in extreme poverty. Another 40% of the healthcare is financed by international donors, meaning that the health care access is to a large degree dependent on where the aid of these donors is focused.
"If targets are to be reached equitably, it is necessary to ensure that well-established patterns of delivering aid do not get in the way of reaching the most vulnerable people" says Mattias Schedwin.
North Kivu, a province in the eastern part of DRC, had the highest health indicator coverage and lowest child mortality. This area has been affected by conflict since the 1990s and has had large humanitarian presence relative to other parts of the country. Additionally, eastern DRC is rich in natural resources and has access to cross-border trade, contributing to the possibility of a larger economy and thereby higher health coverage. On the opposite side, the province Kasaï located in central DRC had the lowest indicator coverage and highest mortality rates. However, this is one of the poorest provinces that furthermore experienced an intense but relatively short conflict episode near in time when data for the study was collected.

Treatment of diarrheal diseases is key
"Our analysis also suggests that preventive, protective and treatment strategies, particularly for diarrheal diseases, could be an effective way to reduce these provincial inequities", says Mattias Schedwin.
Diarrheal disease remains one of the most common causes of mortality for children under the age of five and in the DRC, diarrhoea is estimated to account for 9% of deaths. Great progress has been made in reducing diarrhoeal deaths but during the previous decades, progress has stagnated. The cornerstone for treatment is oral rehydration therapy and zinc. Increasing access is complex and requires an enabling environment with supporting policies, reliable supply chains, as well as provider, and caregiver knowledge and demand.
"In two coming studies, we will take a deeper look at the prerequisites for appropriate treatment of diarrhoeal diseases among care providers in cholera “hotspots” in the DRC. These are the areas where case management should be the best. We hope to identify facilitators and bottlenecks that can help guide future intervention and policy approaches not only in “hotspots” but also on the national level."
New perspectives for future health planning and interventions
"What my study indicates is that, for the DRC, conflict alone is not a good predictor of child health. The reality is more complex. When deciding where to target interventions and health planning you cannot base your judgement only on where conflicts occur because then children outside conflict-affected areas risk being neglected", says Mattias Schedwin.
He draws a parallel to Covid-19 where routine vaccination programs have suffered because of the pandemic. Explaining that as we shift our focus toward what is perceived as most urgent, we risk missing other ongoing challenges.
This perspective is important to the DRC for future intervention roll-out and health system planning to achieve the Sustainable Development Goal 3.2. (end preventable deaths of newborns and children under 5 years of age). Furthermore, it is important to the global discussion about child health and mortality.
"What is important to highlight is that this study looked at the provincial level and lacks insight into the differences within provinces. Hence, it says nothing about children living in the most conflict intense areas nor children in camps for internally displaced persons or refugees.
Nonetheless, the main takeaway from this study is that while addressing the needs of children in conflict-affected areas that often have some of the worst health outcomes, the needs of children in unaffected provinces should not be neglected. We must strive to achieve better health for all children in an equitable way where no one is forgotten", says Mattias Schedwin.
