That's why you feel nausea – and how it can be treated

Chewing gum, acupressure, vaccine. There have been numerous attempts to stop nausea. We have interviewed the researchers who are examining an important revolutionary mechanism that makes us feel sick.
Text: Maja Lundbäck for Medicinsk Vetenskap nr 3, 2023
To feel sick is uncomfortable, and it is supposed to. Food poisoning, infection, cancer treatment and serious exercise. Smell, nervousness, visual impressions and motion sickness. A variety of different things can make us pale and queasy. But how does this occur and why do we react so differently? In order to really find good treatments, researchers need to understand more about the underlying mechanisms behind our nausea. Today, we really do not know how our bodies and minds speak.
However, if the nausea goes so far as to make us throw up, the picture gets clearer. It appears to be almost the same reactions that occur in the body regardless of the trigger. First, signalling molecules are released, either from sensory cells in, for example, the intestines - or from immune cells in tissue and blood. The signals then travel to the brain, for example with the blood via the blood-brain barrier or via nerves from the intestines. Once the signals reach the brain's vomiting centre, information is put together and new signals inform us that we are going to throw up. The reflex is unstoppable, if we must, we must.

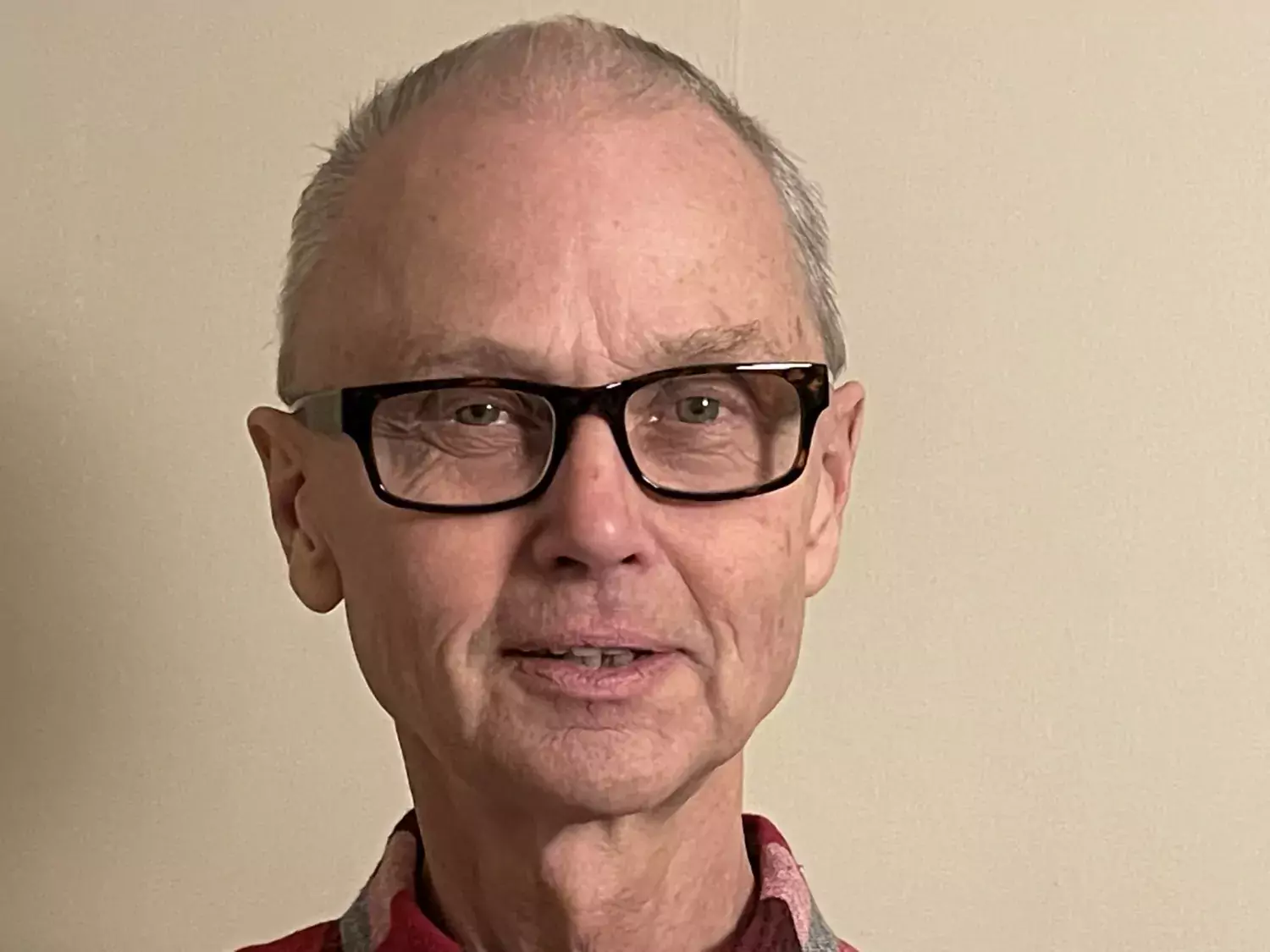
While we are standing there bent over, pushing out our stomach content we may not be thinking that our ability to vomit is basically an evolutionary defence mechanism. But that's how it is. Many animals can also throw up if needed. This is an important function, according to Lennart Svensson, researcher connected to the Department of Medicine, Solna at Karolinska Institutet and Professor Emeritus at Linköping University.
"You should in fact not view nausea and vomiting as something negative. It signals to us that what we are doing is not good. If we go on a carousel and start to feel nauseous we won't want to continue, if we have eaten something bad we will want to throw up," he explains.
Lennart Svensson has conducted research on winter vomiting disease for a long time. The virus does not even time to multiply in the bowel before the signalling molecules have had a chance to inform the brain that it's time to dispose of whatever the brain is interpreting as poison. Cascade vomiting almost always comes before diarrhoea.
"With winter vomiting disease we know that the virus releases serotonin in the bowel, which binds to the gastrointestinal canal's so-called enteric nervous system - and to the vagus nerve, which leads up to the brain," he says.
While vomiting is objective and measurable, nausea is a subjective feeling that may vary in strength - from a vague feeling of discomfort to a sudden need to rid yourself of what is inside of you. You can go around feeling sick for a long time without vomiting.

Women are more easily disgusted
We humans also have weak stomachs, which is both connected to environment, genetics and dependency, according to Supreet Saluja, who has a post-doctoral position at the Department of Clinical Neuroscience at Karolinska Institutet.
Some people feel disgusted and somewhat ready to throw up just from the thought of, for example, faeces - or contagious disease.
"Typically, women are more easily disgusted, at least when it comes to picturing how disgusting something can be," she says.
The same brain area that is involved in processing pain and evaluation of threats, a section called insular cortex, is also believed to be involved in the experience of disgust. But exactly what occurs in the brain is unexplored.
Not only how easily you feel disgusted but also how the disgust alarms us varies. During the pandemic, when we were all advised to wash our hands more carefully - since there was a real threat - the number of people with OCD-like symptoms also increased among the entire population. OCD means obesessive compulsive disorder and individuals with a sub-type of OCD may be scared to touch door handles or perceive clean things as contaminated.
"Individuals with OCD may feel relief when they wash their hands or spend time doing other hygiene-related behaviours," says Supreet Saluja.
Feelings of disgust in individual with OCD are not as easily treated as with traditional exposure therapy. Two other treatments might help though - one method involves presenting, for example, a door handle together with a pleasant smell. The other involves thinking that things that you need to touch are not only gross and negative, but that they also have a positive function," she explains.
The vulnerability to disgust is not stable over time, we often become less easily disgusted as we age.
"And studies on medical students, who have been followed over time, show that disgust over dead bodies and bodily fluids decreases dramatically during their training," she says.
At leasts that is what the students report. However, there are challenges to studying subjective experiences. Another example is investigations into how many people suffer postoperative nausea. Do you only count those who vomit, those who feel nauseous but do not vomit — or do you also include those who only feel vaguely nauseous?
It is well known that it is common to feel nauseous after surgery under narcosis. Exactly what triggers this nausea is unclear, but we do know that the longer you are under narcosis the higher the risk is that we experience nausea. The longer the operation, the greater the risk of nausea.
An increase in abdominal surgery and surgery on breasts or ears-nose-throat has been noted, as well as in plastic surgery. Studies also show that women, people under the age of 50 and people who have previously experience nausea during surgery and non-smokers have an increased risk. Surgeries that are associated with more pain after the surgery and higher doses of painkillers may also cause more nausea.
Jan Jakobsson, adjunct lecturer at the Department of Clinical Science, Danderyd Hospital, the Department of Anaesthesia and Intensive Care, has long been attempting to find out how you can prevent nausea in patients who have been operated under narcosis.
A couple of years ago, Jan Jakobsson and his colleagues showed that women who have undergone a gallbladder operation and have received a nutrition beverage before the operation and a chewing gum shortly after waking up recovered considerably faster compared to a control group.
"Custom-made narcosis, so that the doses of the narcosis agent do not become too high, but also using non-opioid painkillers as much as possible, has also be shown to reduce the risk. Although there are no guarantees to avoiding postoperative nausea," says Jan Jakobsson.
Overall it has been difficult to produce really good active substances and treatments against nausea - regardless of whether it involves trying to combat postoperative nausea, intestines or a disturbed sense of balance.
"There is not one single drug that removes all symptoms," says Lennart Svensson.
There are several drugs that block different signalling paths that can induce nausea, such as serotonin receptor blockers or substance P blockers, which are used with chemotherapy. But no drug can put a stop to any type of nausea.
Unclear how to treat pregnancy nausea
Another condition that causes nausea is pregnancy. With extreme pregnancy nausea you currently use drugs that are used for other nausea conditions, such as histamine blockers. The problem is that not everyone is helped by this. We are currently not sure what treatment is the most effective on pregnant women. To answer that question, the Swedish Agency for Health Technology Assessment and Assessment of Social Services conducting an investigation last year. They came to the conclusion that there is no answer to that question.

"The studies that are available are too small and too few and have low reliability. We observed a tendency that acupressure in combination with standard care, thus anti-nausea drugs, might be effective, that's all, says Hanna Ulfsdottir, midwife and assistant lecturer at the Department of Women's and Children's Health at Karolinska Institutet, and one of the experts in the SBU investigation.
One reason for why one was not able to produce more well-founded results is that the international definition of extreme pregnancy nausea was not introduced until 2021. Without a definition it is difficult to compare studies. It has now been established that extreme pregnancy nausea entails: Symptoms before pregnancy week 16, with nausea and vomiting, of which at least one is of a serious degree, inability to eat or drink normally and serious limitation of daily activities.
"The fact that there is now a definition helps. Now treatments can be compared with each other," says Hanna Ulfsdottir.
Since a common definition has not existed, it is also unclear how many women actually suffer from this, but somewhere between 0.3 and 3 percent of all pregnant women think that they feel this sick. Extreme pregnancy nausea results in major social costs. In 2021, 5,600 pregnant women were on sick leave due to vomiting, 3,300 of them were on sick leave for at least 60 days. Many women are also so dehydrated that they need IV treatment in hospital.
"There is a lot of suffering here, there are studies that show that women terminate their pregnancy because they cannot stand it or abstain from having more children - and yet we know very little about why some women are hit so hard," she explains.
"A lot indicates that there is a link to pregnancy hormones, especially HCG, the hormone that is measured in pregnancy tests. Twin pregnancies, where HCG levels are higher, often cause more nausea," says Hanna Ulfsdottir
It is also believed that psychosocial and genetic factors can play a role," she explains.
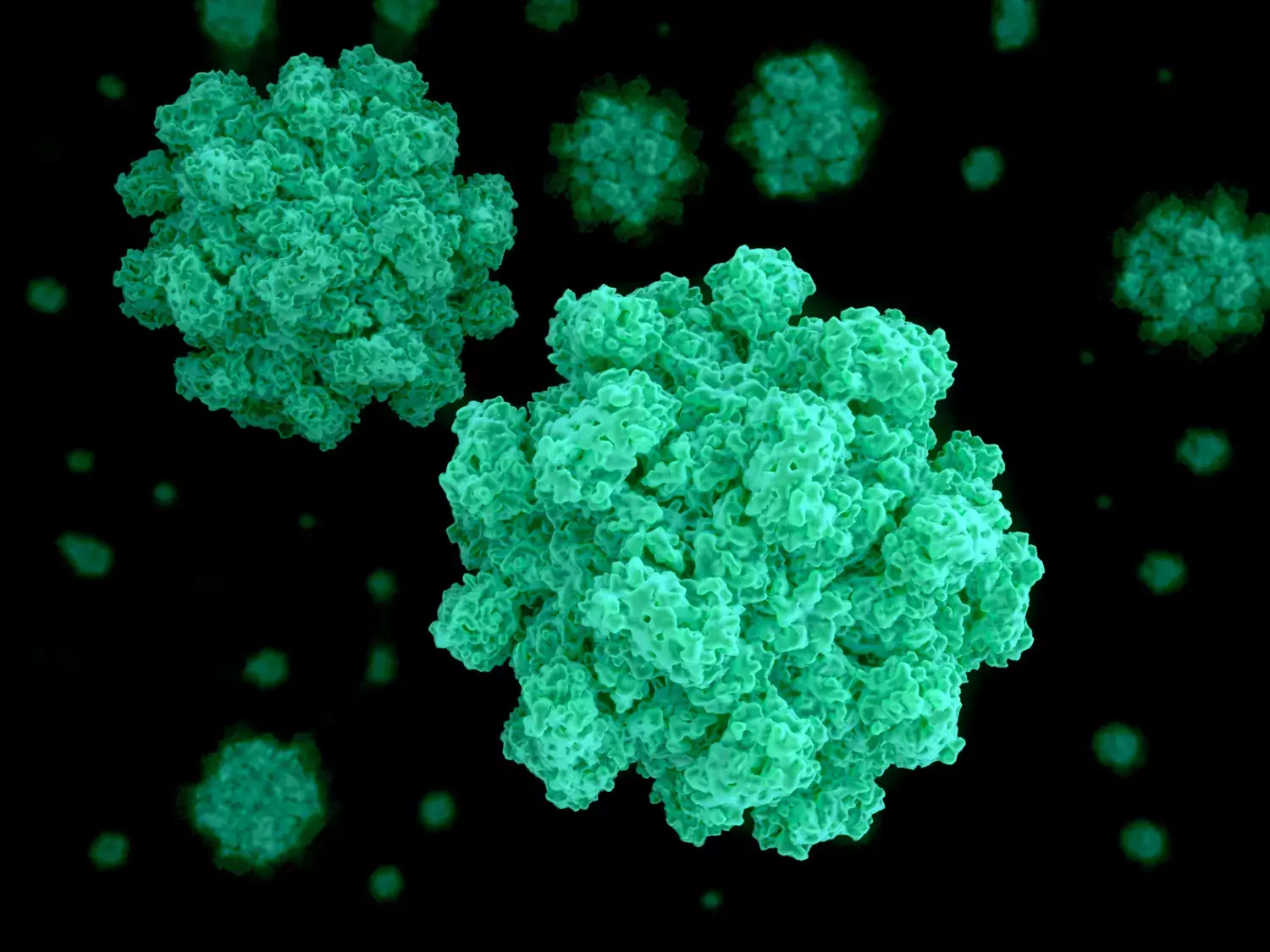
Mutation protects against winter vomiting disease
With winter vomiting disease - which in 80 percent of cases is caused by norovirus - we know that genetics plays an important part. Most people get sick from norovirus, but not everyone. Some of us lack the cell receptor for the virus. That means that you can not get infected nor spread the virus to other people.
"A mutation in the enzyme FUT2 in chromosome 19 pretty much protects against infection if you have two mutated gene copies," says Lennart Svensson.
The mutation, which one out of five westerners carry, is most likely at least 40, 000 years old and protects against the most common novovirus stem.
The fact that a vaccine against winter vomiting disease would please everyone is something that a lot of people can agree on.
However, finding a vaccine has not been easy. That should perhaps not be considered that strange, since not even the natural immunity lasts very long, the virus exists in many variants - and it is also mutable. Researchers have been trying and failing time and time again.
"However, there are currently four possible vaccines being developed. The ones that have progressed the furthest are protein based vaccines that are administered either orally or as an injection. They provide a strong immune system, but it is unclear whether they actually protect against illness," says Lennart Svensson.
Three facts you (most likely) did not know about winter vomiting disease
- 200,000 people die worldwide from winter vomiting disease every year due to dehydration.
- Women with a mutation that makes them immune to winter vomiting disease are also at an increased risk of urinary tract infection.
- 20 percent of winter vomiting disease is caused by sapovirus, which the mutation does not protect against.
Source: Lennart Svensson
About the magazine Medicinsk Vetenskap
 Photo: Jens Magnusson
Photo: Jens MagnussonRead more articles about medical research
Read about the latest in medical science in Karolinska Institutet's Swedish language popular science magazine Medicinsk Vetenskap. Subscribe now!
