Specialized immune cells compensate for a leaky blood nerve-barrier
Harald Lund, Matthew Hunt, Zerina Kurtović & Camilla Svensson have published an article in the Journal of Experimental Medicine. They have discovered a unique structure in the blood-nerve barrier in a region of the peripheral nervous system called the dorsal root ganglia (DRG). The study has implications for understanding how diseases target the nervous system and how they can be treated.
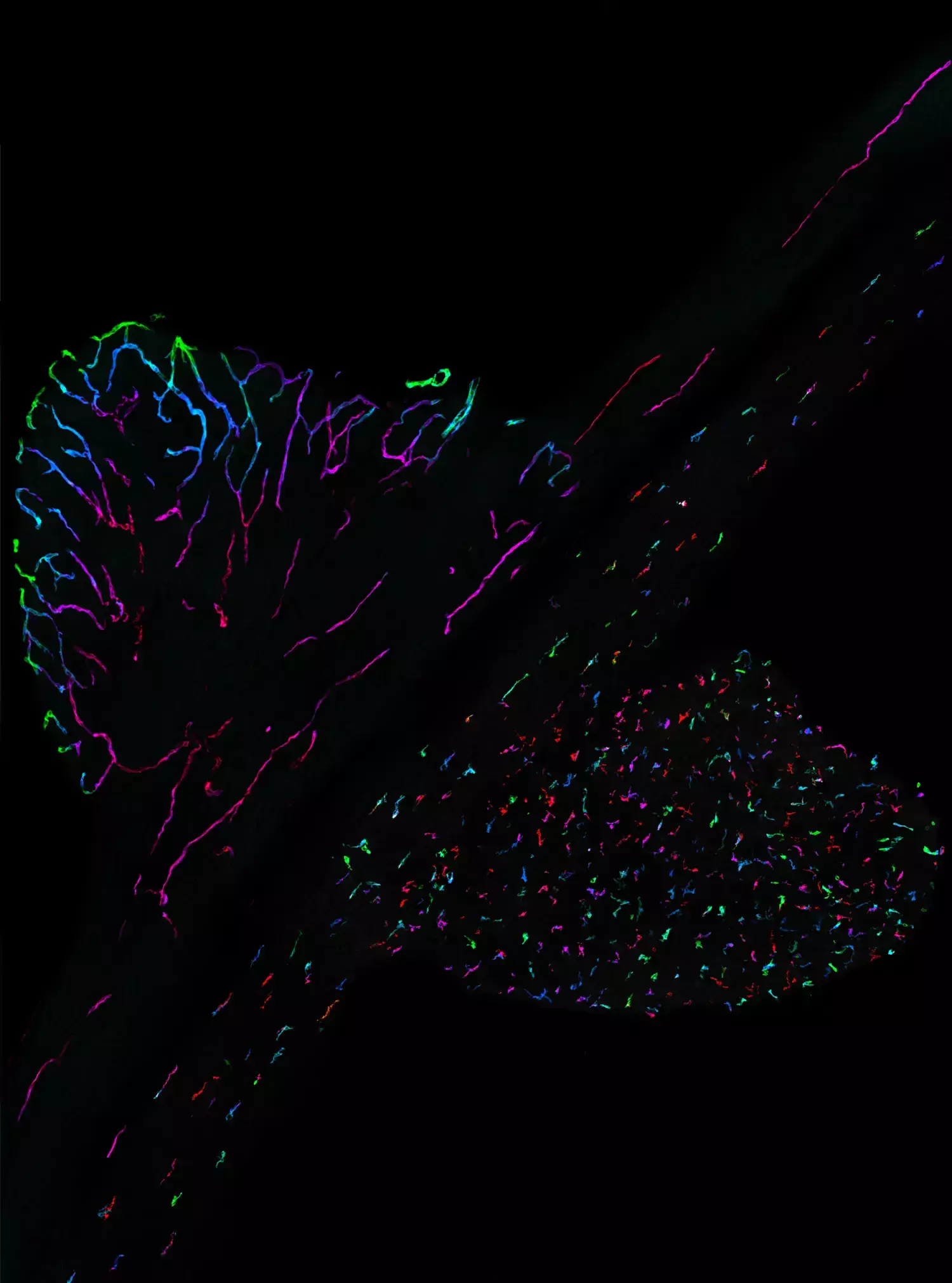
The blood vessels in the peripheral nervous system are impermeable, which prevents toxic molecules or pathogens in the blood from gaining access to the nervous system. This makes up the so called blood-nerve barrier. By mapping the blood-nerve barrier Camilla Svensson’s research group has discovered an increased permeability in a region called the dorsal root ganglia (DRG). The blood vessels in DRG are covered by a unique network of macrophages, a type of immune cell, that compensates the increased permeability by taking up proteins and molecules from the blood.
Why are the results important?
1. Sensitivity to toxic molecules: DRG-neurons are particularly sensitive to toxic molecules in the blood, such as chemotherapy, which can lead to pain and sensory disturbances, a condition called chemotherapy-induced peripheral neuropathy. The increased permeability of the blood-nerve barrier is likely a biological explanation for this phenomenon.
2. Possibility to deliver therapeutic drugs: The leaky blood-nerve barrier in the DRG provides an opportunity to efficiently deliver drugs into the nervous system.
3. Compensatory system: The study shows how the nervous system has developed a compensatory system through an active immune defense, the macrophages, to handle the increased permeability of the blood-nerve barrier.
How was the study performed?
When they discovered that the blood vessels in the DRG were covered by a type of macrophage network, they decided to study the system in more detail. They have made use of techniques such as single-cell RNA-sequencing, flow cytometry, immunohistochemistry and functional studies.
What is the next step in your research?
The next step in their research is focused on manipulating the blood-nerve barrier in different ways. For example by increasing or decreasing the permeability of endothelial cells (the cells that make up the blood vessel wall) or by altering the activity or the number of macrophages.
- We are particularly interested in understanding how the nervous systems’ vulnerability to chemotherapy can be affected by these manipulations, says Harald.

For how long have you been working on this project?
Matthew and Harald met in San Diego five years ago, during Harald’s first postdoc. This is where they came up with the project idea and where they performed the first experiments. The two researchers subsequently moved to Camilla’s lab, where Zerina had started as a PhD student. Together they have spent three years actively researching the project in Camilla’s lab. Harald, Matthew and Zerina share the first name authorship on the article.
What is the most fun part about doing research?
In an interview, Harald describes what he enjoys most about the research. He explains that a large part of the project involves dissecting tissues from mice, followed by sectioning and staining with antibodies before they are placed under a microscope. Harald points out that reaching this stage takes a lot of work, “so when you find yourself at the microscope and realize that the experiment has worked, it’s an amazing feeling”.
Matthew adds that after a successful experiment, you send pictures to the rest of the group to share the feeling with your lab members.
