Oxidative stress in heart failure varies between males and females
Researchers from Karolinska Institutet, AstraZeneca, Würzburg University, Science for Life Laboratories and Uppsala University have found that oxidative stress in heart failure varies depending on sex, with female mouse hearts having stronger natural defenses against oxidative damage. The study could enable new approaches for precision medicine and may explain why previous attempts to use antioxidants for treating heart failure have not been so successful.
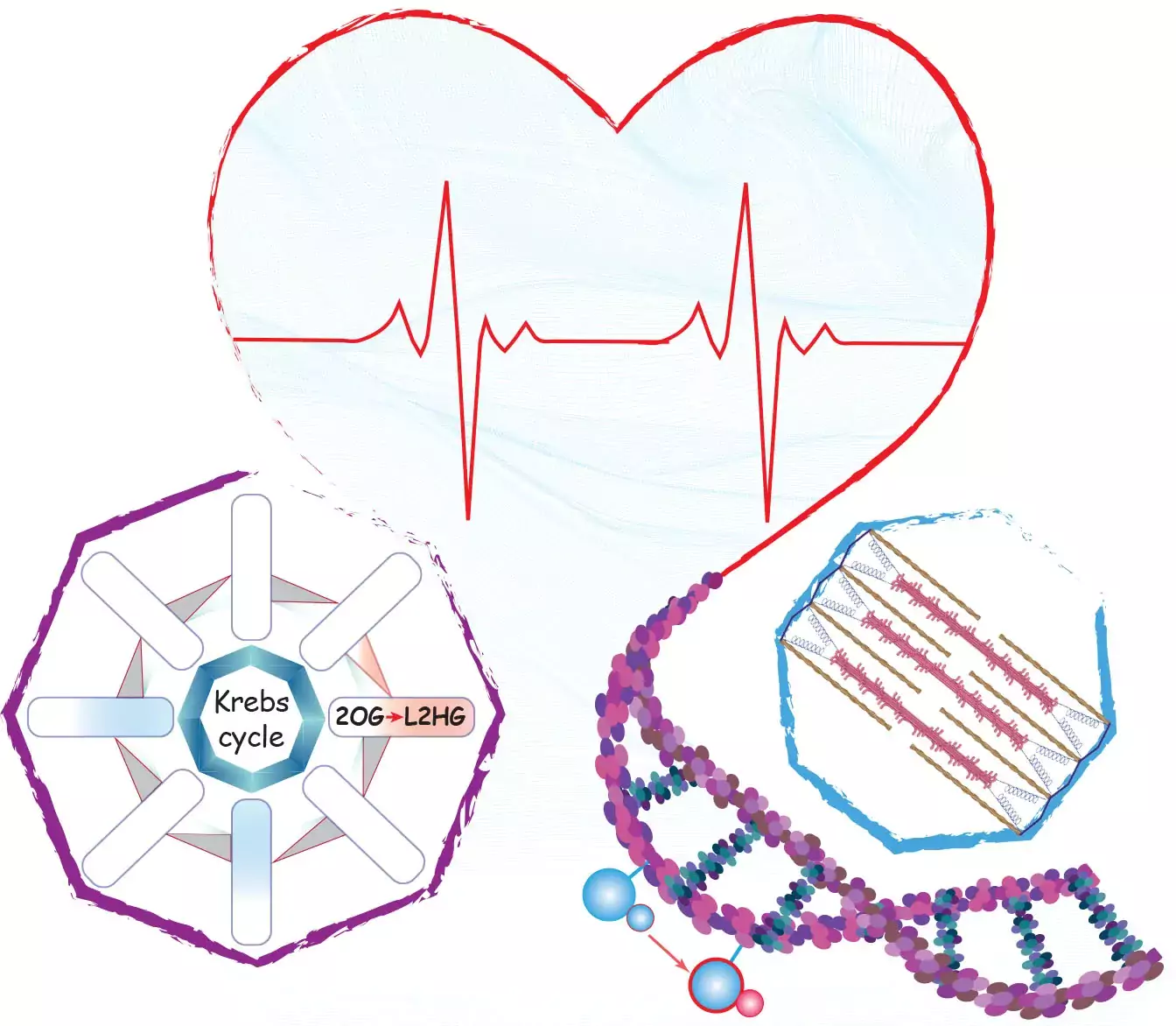
The study published in Nature Communications, was led by Zaher Elbeck in Professor Christer Betsholtz research group at the Department of Medicine, Huddinge (MedH) and reveals the important roles of two proteins, IDH2 (isocitrate dehydrogenase 2) and NRF2 (Nuclear factor erythroid 2-related factor 2), in shielding the heart from oxidative damage through a mechanism involving mitochondrial-nuclear metabolites.
The study used a multi-pronged approach, analyzing metabolites, gene expression, and epigenetics, in mouse and human heart tissue samples, alongside the analysis of large public databases. A number of innovative methods were also developed to precisely measure the heart's natural antioxidant capacity. Upon identifying unique regulation of IDH2 expression, researchers explored its underlying antioxidative mechanism and key molecules using human heart cells and animal models. Testing a novel AstraZeneca experimental compound in a murine heart failure model further revealed potential for targeted and effective antioxidative treatment.
Results emphasises need for personalized treatments
Female murine hearts demonstrated superior antioxidative capacity compared to males. Targeting oxidative stress in a murine model of heart failure improved heart function only in males, whereas females, which typically possess sufficient innate antioxidative capacity, experienced adverse effects from the treatment. These results emphasize the need for “personalized” antioxidant therapies in heart failure, that consider individual antioxidant levels.
The heart's natural robust antioxidative defense
¨Previous attempts to treat heart failure and other diseases using antioxidants have generally seen limited success. Our study identifies some existing misconceptions in the field and reveals a possible reason for the lack of druggability: the heart's natural robust antioxidative defense¨, says Zaher Elbeck.
The study findings challenge past notions by highlighting the heart's robust natural antioxidative defense and distinguishing between conditions of oxidative stress and oxidative damage.
Free radicals part of normal biological reactions
Oxidative stress happens when our cells break down nutrients to create energy and building blocks for cell function, as part of normal biological reactions. These reactions also generate free radicals, which can harm our cells if uncontrolled. Our cells have strong natural defenses against these radicals, but in a disease state, such as in heart failure, this defense may be insufficient. When the cell's ability to handle these free radicals weakens, it can cause stress on the cell, known as oxidative stress, and eventually lead to oxidative damage. Additionally, certain important biological functions in our cells require a low level of free radicals to operate effectively and maintaining adequate levels of free radicals is also essential.
Though oxidative stress occurs in heart failure, most heart cells possess adequate antioxidants to ameliorate and prevent oxidative damage. The challenge is that battling oxidative stress is metabolically demanding, especially in failing hearts with energy and metabolic deficiencies. Thus, personalized antioxidant therapy, based on individual antioxidant levels assessed through biomarkers, could support more effective treatment and management.
Precision medicine and antioxidative therapies
Dilated cardiomyopathy is a condition where the heart chambers become enlarged and the pumping capacity of blood decreases and becomes insufficient, especially during physical exercise. It is a common heart disease in men, but it can also happen to women as they get older.
This study set out to understand how sex differences influence oxidative stress in dilated cardiomyopathy. Our findings provide valuable insights to improve heart failure treatments, emphasizing the potential opportunity for a precision medicine approach in designing effective antioxidative therapies. Future efforts will concentrate on developing specific biomarkers for antioxidative capacity assessment and therapeutic targets for precision medicine.
The study was conducted in collaboration with AstraZeneca, University of Würzburg, Science for Life Laboratories and Uppsala University and funded by AstraZeneca.
Publication
ElBeck, Z., Hossain, M.B., Siga, H. et al. Nat Commun 15, 2358 (2024).
